Views: 3
– The initial battle takes place in the nostrils, the study indicates alternative pathways that the virus can use to enter the lungs, central nervous system and heart
Minapim by Hernan Valenzuela: In several studies, scientists at Cornell University have identified the cunning behavior of SARS-CoV-2, which causes the COVID-19 coronavirus. When the virus enters the body, it shuts down a part of the immune system, facilitating its spread within the body for a few days before the immune system can identify the invader.
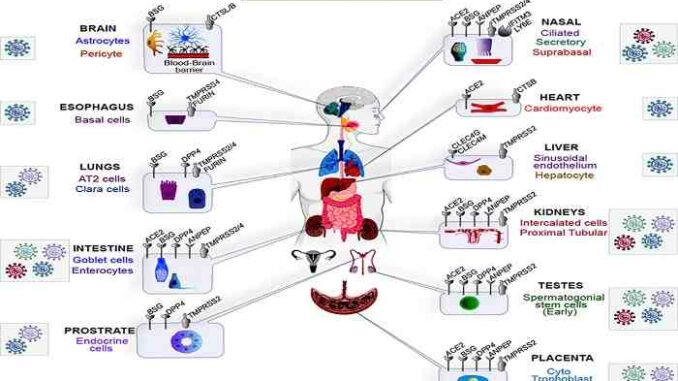
The researchers have yet to identify the full scope of tissues and cell types that are most vulnerable to SARS-CoV-2. Much research has focused on identifying genes and pathways that facilitate entry of the virus into lung cells, but clinical and scientific data indicate that it can cause damage to a wide range of organs.
In new research at Cornell University, potential roadmaps for the internal process of the virus were developed, in the infection of other organs and identifies which molecular factors can help to facilitate or restrict the infection.
To predict the growth (tropism) of the human coronavirus, 28 SARS-CoV-2 and coronavirus-associated receptors and factors (SCARFs) were profiled using transcriptomics (studies the RNA molecules, which determine which genes will be expressed) a single cell in several healthy human tissues. SCARFs include cellular factors that facilitate and restrict viral entry.
“The data suggest that it is not just a respiratory disease. It is much broader than that and has the potential to affect many other organs, ”said Cedric Feschotte, professor in the Department of Molecular Biology and Genetics at the Faculty of Agriculture and Life Sciences. “Our analysis suggests that there is a wide range of cellular vulnerabilities.”
Feschotte is the lead author of “A Single Cell RNA Expression Map of Human Coronavirus Input Factors” in Cell Reports. Other co-authors are Manvendra Singh, a postdoctoral associate at Feschotte Lab and a Cornell Presidential Fellow; and Vikas Bansal, computational biologist at the German Center for Neurodegenerative Diseases in Bonn.
The new study maps the expression of 28 human genes called “SCARFs” – SARS-CoV-2 and Receptors and Factors Associated with Coronavirus action. By looking at the RNA expression of a single cell in these genes, they can predict which tissues and cell types are most vulnerable to infection by the action of the coronavirus – in adults and embryos.
The analysis also predicts entry paths that do not follow the most usual structure for lung and brain infections. Sperm cells and prostate endocrine cells also appear to be permissive to SARS-CoV-2 infection, suggesting male-specific vulnerabilities.
Both pro and antiviral factors are highly expressed in the nostrils (in the nasal epithelium), with potential age-dependent variation, providing an important battleground to stop infection by the action of the coronavirus. The analysis also suggests that early embryonic and placental development has a moderate risk of infection.
Finally, the expression SCARF appears to be largely conserved in a subset of primate organs examined. The study establishes a resource for investigations into coronavirus biology and pathology.
“You can learn which cells and organs are most likely to be infected – at least at the beginning of an infection,” said Feschotte. “It is very important to emphasize this, because once the virus infects a certain tissue, the [genetic] scenario can change.”
Without the ability of the immune system to respond quickly, said Feschotte, naturally occurring restriction factors already present in tissues represent the body’s main line of defense against SARS-CoV-2.
Mapping the different points of entry for the virus is also essential in trying to predict where the virus will go after entering the body. In addition, by identifying the molecular routes of infection, other researchers can use these areas as targets for developing drugs to overcome the infection.
The study indicates alternative pathways of entry for how the virus can enter the lungs, central nervous system and heart. His research also supports emerging clinical data showing that SARS-CoV-2 also infects the intestines, kidneys and placenta.
They noted that specific groups of cells within the prostate and testicles are likely to be permissive for SARS-CoV-2 and may help explain male-specific vulnerabilities.
In addition, this study increases researchers’ knowledge of what happens when the virus interacts with nasal tissues, an access point for the virus to enter.
The team reported that the tissue on the roof of the nasal canal, called the nasal epithelium, appears as crucial battlefield between the virus and the nasal cells, because this tissue shows high expression of genes that both facilitate and restrict infection.
The researchers believe that the outcome of the nasal battle can be critical in determining the course of an infection. Interestingly, they also observed a statistical difference in the level of expression of these factors of entry into the nasal tissue of younger people (under 30) versus older people (over 50).
“There were significantly more nasal cells expressing SARS-CoV-2 input factors in older people than in young people,” said Singh. Although the sample size of the group was too small to draw a firm conclusion, he said, if this trend continues in larger cohorts, then “this could, in part, explain why older people are getting sicker than young people” .
The other crucial organ is the placenta.
“We found that placental cells called trophoblasts appear to be vulnerable,” he said. “It is frightening to think that if the placenta can be infected, the virus can infect other fetal tissues, with harmful consequences for the health of the fetus, as seen with the Zika virus.”
Feschotte noted that the placenta may still prevent newborns from being infected while they are in the womb. Current studies suggest that transmission between infected mothers and their babies during the third trimester of pregnancy is very rare. But he emphasized that it is still too early to say whether there is a greater risk of transmission in the early stages of pregnancy and what consequences this may have on fetal development.
As part of this project, the team also developed a friendly, open-access web interface, where anyone can search for RNA expression from a single SCARF cell. This will facilitate access to data that will help scientists around the world.
“This is a useful resource for COVID-19, but perhaps also for the next coronavirus pandemic; not that I want one, ”said Feschotte. “But we have to be realistic and better prepared. Part of being prepared is having the data available. “
Highlights
- SCARF single cell transcriptome profile in various somatic and reproductive tissues
- Intestine, kidneys, placenta and spermatogonia seem more permissive for coronavirus
- The nasal epithelium exhibits high expression of promoting and restrictive factors
- SCARF expression is conserved in the main human organs, chimpanzees and monkeys
The work at Feschotte Lab on host-virus interaction is funded by the National Institutes of Health.
Sources: Cornell University Jana Wiegand Cell reports
Related article: Blood type “O” protects you from coronavirus – Norway discover