Views: 6
– Cancer cells are killed in lab experiments and tumour growth reduced in mice, using a new approach that turns a nanoparticle into a ‘Trojan horse’ that causes cancer cells to self-destruct, without using drugs, a research team at the Nanyang Technological University, Singapore (NTU Singapore) has found.
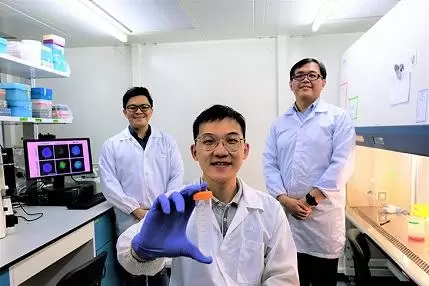
Courtesy NTU: The researchers created their Trojan horse nanoparticle by coating it with a specific amino acid – L-phenylalanine – that cancer cells rely on, along with other similar amino acids, to survive and grow. L-phenylalanine is known as an ‘essential’ amino acid as it cannot be made by the body and must be absorbed from food, typically from meat and dairy products.
Studies by other research teams have shown that cancer tumour growth can be slowed or prevented by ‘starving’ cancer cells of amino acids. Scientists believe that depriving cancer cells of amino acids, for example through fasting or through special diets lacking in protein, may be viable ways to treat cancer.
However, such strict dietary regimes would not be suitable for all patients, including those at risk of malnutrition or those with cachexia – a condition arising from chronic illness that causes extreme weight and muscle loss. Furthermore, compliance with the regimes would be very challenging for many patients.
Seeking to exploit the amino acid dependency of cancer cells but avoid the challenges of strict dietary regimes, the NTU researchers devised a novel alternative approach.
They took a silica nanoparticle designated as ‘Generally Recognized As Safe’ by the US Food and Drug Administration and coated it with L-phenylalanine, and found that in lab tests with mice it killed cancer cells effectively and very specifically, by causing them to self-destruct.
The anti-cancer therapeutic nanoparticle is ultrasmall, with a diameter of 30 nanometres, or approximately 30,000 times smaller than a strand of human hair, and is named “Nanoscopic phenylalanine Porous Amino Acid Mimic”, or Nano-pPAAM,
Their findings, published recently in the scientific journal Small, may hold promise for future design of nanotherapies, said the research team.
Assistant Professor Dalton Tay from the School of Materials Science and Engineering, lead author of the study, said: “Against conventional wisdom, our approach involved using the nanomaterial as a drug instead as a drug-carrier. Here, the cancer-selective and killing properties of Nano-pPAAM are intrinsic and do not need to be ‘activated’ by any external stimuli. The amino acid L-phenylalanine acts as a ‘trojan horse’ – a cloak to mask the nanotherapeutic on the inside.”
“By removing the drug component, we have effectively simplified the nanomedicine formulation and may overcome the numerous technological hurdles that are hindering the bench-to-bedside translation of drug-based nanomedicine.”
Intrinsic anti-cancer therapeutic properties of Nano-pPAAM
As a proof of concept, the scientists tested the efficacy of Nano-pPAAM in the lab and in mice and found that the nanoparticle killed about 80 per cent of breast, skin, and gastric cancer cells, which is comparable to conventional chemotherapeutic drugs like Cisplatin. Tumour growth in mice with human triple negative breast cancer cells was also significantly reduced compared to control models.
Further investigations showed that the amino acid coating of Nano-pPAAM helped the nanoparticle to enter the cancer cells through the amino acid transporter cell LAT1. Once inside the cancer cells, Nano-pPAAM stimulates excessive reactive oxygen species (ROS) production – a type of reactive molecule in the body – causing cancer cells to self-destruct while remaining harmless to the healthy cells.
Co-author Associate Professor Tan Nguan Soon from NTU’s Lee Kong Chian School of Medicine said: “With current chemotherapy drug treatment, a common issue faced is that recurrent cancer becomes resistant to the drug. Our strategy does not involve the use of any pharmacological drugs but relies on the nanoparticles’ unique properties to release catastrophic level of reactive oxygen species (ROS) to kill cancer cells.”
Providing an independent view, Associate Professor Tan Ern Yu, a breast cancer specialist at Tan Tock Seng Hospital said, “This novel approach could hold much promise for cancer cells that have failed to respond to conventional treatment like chemotherapy. Such cancers often have evolved mechanisms of resistance to the drugs currently in use, rendering them ineffective.
However, the cancer cells could potentially still be susceptible to the ‘Trojan horse’ approach since it acts through a completely different mechanism – one that the cells will not have adapted to.”
The scientists are now looking to further refine the design and chemistry of the Nano-pPAAM to make it more precise in targeting specific cancer types and achieve higher therapeutic efficacy.
This includes combining their method with other therapies such as immunotherapy which uses the body’s immune system to fight cancer.
Ref: “Potent‐By‐Design: Amino Acids Mimicking Porous Nanotherapeutics with Intrinsic Anticancer Targeting Properties“, published in Small, 19 July 2020.
Related article: Using AI to understand the spread of cancer