
Views: 23
– It is better for health to be active and slightly overweight – “fit and fat” – than sedentary and slender. Why that? UiO researchers are facing a broad alliance that will develop better treatments for diabetes and overweight, which are the leading and growing public diseases.
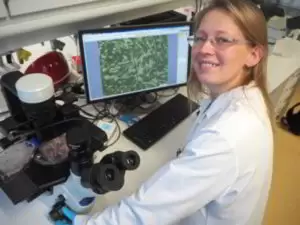
Courtesy Oslo University by Bjarne Rosjo: Good treatments for obesity and diabetes, which are important and growing public diseases, are lacking. However, researcher Eili Tranheim Kase has a plan: “We can make great strides when academia and the pharmaceutical industry work together – and if we shorten the path of basic research to applied medicine,” she says.
Obesity and diabetes are two “breeding horses” that are becoming increasingly social problems. More than a third of the world’s 7.7 billion people are obese, and about one in five develop type 2 diabetes in their lifetime. Type 2 diabetes develops over time and causes few symptoms at first, but eventually the disease leads to high blood sugar – which in turn can create a number of new problems.
The biggest problem with type 2 diabetes is that the disease dramatically increases the risk of cardiovascular disease, stroke, eye disease, kidney damage, liver damage, dental disease, erectile dysfunction and more. Therefore, it is about reducing the risk of people being affected by this disease. In addition, there is a strong need to develop new drugs that can provide better help to those who have already developed type 2 diabetes, says Eili Tranheim Kase in the UiO Department of Pharmacy.
Better medication, faster results
About 200,000 people with type 2 diabetes have been registered in Norway, and many people are likely to continue unknowingly. I start quite frightening, and most people are not diagnosed until the disease gets so far that the resulting damage begins to occur.
Researchers at the Department of Pharmaceuticals have been working for many years to explore the possibilities of developing new type 2 diabetes drugs.
– The first one we will develop will be a new model for testing possible new drugs so we can shorten the path from basic research to final medicine. The second is that we should focus more on collaboration with the pharmaceutical industry, she says.
Collaboration with industry
In 2016, the Institute of Pharmaceuticals signed a cooperation agreement with the British-Swedish pharmaceutical company Astra Zeneca, which has approximately 65 employees in Norway and more than 50,000 employees internationally. Pharmacists have also come to terms with four small start-ups and entrepreneurs.
There has been a lot of research on diabetes in academia and business, at least since I do research. But developing new medicines is extremely laborious. Therefore, it is obvious that we should cooperate more so that we can better leverage the competence and overall resources of academia and industry. I am convinced that this must be the future in the development of new medicines, ”says Kase.
Eili Tranheim Kase is now coordinating a request that has been submitted to the Norwegian Research Council. The four research institutions and the five companies behind the proposal want to become a Research Oriented Innovation Center (SFI). If your proposal is approved, the Research Council will provide a generous grant spread over a period of up to eight years.
There is fierce competition from SFI funds, as up to 70 applications were received before the deadline expired in September.
– There will hardly be more than 10 to 12 proposals awarded. But we have a good chance and we promise a lot of groundbreaking work and broad cooperation if we become one of the groups receiving an SFI grant. The hope is that we can create a center that can help build a new Norwegian business community that can also gain access to international markets, says Kase.
Three dimensional test
If the SFI request is granted, the new CIP-OD center will focus on developing a new model for drug testing. Today, it takes a long time to come from basic research and good ideas for a finished drug that can reduce the risk of developing type 2 diabetes – or alleviate symptoms if the disease is first developed.
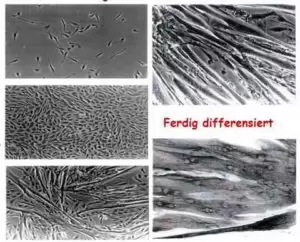
– The first step in testing a new drug is to investigate how it works in vitro, ie in cells grown in a glass container in the laboratory. Then we can test in vivo – on live animals – before finally testing how medicines work on humans. This all takes many years, says Kase.
In the new center with SFI, Kase and its partners want to further develop the way in vitro testing is done today.
– Today, this test is usually done on muscle cells, fat cells or liver cells that grow in very thin layers, so in principle the test takes place in two dimensions (2D). But the cells of living animals and humans do not live in two dimensions, but in three! That’s why we want to develop a model that allows us to test how drugs work in thicker layers of cells, in three dimensions (3D), says Kase.
– This will give us better results than current 2D models and probably saves a lot of time because we don’t have to go back to the beginning as often as we do today. We spend a lot of time studying drug candidates, and then it doesn’t work, she adds.
The advantage of being “fit and fat”
We still don’t know much about why someone develops type 2 diabetes, but researchers have noted a number of relationships that are not well known among most people. For example, why only one in five overweight people develop the disease while the other four manage it well?
It is well documented that it is more dangerous to be inactive and thin than to be active and slightly overweight! In the countryside, many talk about being “fit and fat,” as are many Norwegians. In Norway, many people are overweight and are active, among other things, walking or walking on weekends, says Kase.
“But Americans laugh at us when we talk about it, because the ‘fit and fat’ group doesn’t exist in the United States.” There, people are very inactive and drive cars everywhere, while those who are active are really very active. Instead, we Norwegians are often a little more “in the middle of the tree”, overweight and active. It’s very good training if you weigh 10 to 15 pounds more and take a long uphill hike up the mountain, she points out.
The Mechanisms Behind Diabetes

Type 1 and 2 Diabetes
- Type 2 diabetes occurs most often in adults and you are very likely to suffer from it if your parents have it. But it is also the case that being overweight and having a healthy life – such as unfavorable diet, little exercise and smoking – increases the risk of developing the disease.
- Type 1 diabetes, on the other hand, can begin in all age groups, most often in children, adolescents and adults under 40 years. The disease is hereditary and there are many unanswered questions about why anyone has type 1 diabetes.
Researchers from the Department of Pharmacists have observed what happens in your body and cells when you exercise is very similar to what happens when insulin activates muscle and fat cells after a meal. After all, there are two different mechanisms for judging, but both cause cells to absorb more glucose from the bloodstream.
So you can imagine that you can develop diabetes medications that “mimic” some of the effects you get from exercise. In that case, it would be a big step for the group that has become so overweight that they can no longer exercise, Kase suggests.
Insulin-producing cells reside in the pancreas, and in healthy individuals, these cells begin to produce insulin immediately after a carbohydrate-rich meal. Insulin enters the bloodstream and reaches the cells, where it causes rapid absorption, storage and use of glucose in most body tissues – but especially in the muscles, fat and liver.
In some people who move very little while eating, over time the cells in body tissues gradually become less sensitive to insulin. We say they develop insulin resistance, and then the pancreas reacts with increased insulin secretion in the blood – and then glucose uptake increases anyway. I usually tell students that it’s almost as if our cells are deaf: so the insulin should scream louder than, “Now it’s sugar here!”
But that only works for a while, because if you’re heavy today, you’re probably even heavier tomorrow – or at least a year. Increased insulin production causes the pancreas B cells to wear out and eventually die.
That’s when people develop type 2 diabetes, because insulin production fails. So sugar is doesn’t more absorbed by cells but remains in the bloodstream. And then sugar can cause all kinds of diseases and cause all the diseases we talked about earlier, says Kase.
In practice, this means that many people can walk for years with incipient type 2 diabetes without realizing it. It also doesn’t help to go to the doctor and measure blood glucose level, because glucose is normal until insulin-producing cells no longer function.
– This condition could have been detected if the doctor measured the level of insulin in the blood. But it’s a more expensive and complicated analysis that’s not common in GP, says Kase.
Immigrants at Risk
The risk of developing insulin resistance is not equally distributed worldwide. Most ethnic Norwegians gain a few pounds without falling into the danger zone, but in some other parts of the world, it takes a little overweight before people develop insulin resistance.
Perhaps this is why many immigrants from warmer regions, particularly Asia and Africa, become type 2 diabetics within a few years of moving to Norway. In 2017, the National Institute of Public Health presented statistics showing that diabetes is prevalent among immigrants from Sri Lanka, India and Pakistan. Here, 20-24% of adults aged 30-59 have diabetes, compared with 3-6% of the population in Norway.
The increasing number of diabetics in parts of the immigrant population is probably not only due to genetics, but also to a less active lifestyle than the original Norwegian population. The fact that ethnic Norwegians can tolerate more obesity may be due to the fact that there was a special group that settled and survived in our cold and inhospitable regions when Norway was populated after the last Ice Age.
Not for many generations, for it made sense to put on weight in summer and fall so that the traffic industry could continue with the cold, harsh Nordic winter. Today, however, it is no longer so smart to get fat in the summer, because we have equally good access to food, even in winter, Kase points out.
Project partners
The new center will be named Innovative Pharmacological Research Center for Obesity and Diabetes if the SFI application is granted. The center currently has nine partners:
- Department of Pharmacy, University of Oslo,
- Oslo University Hospital,
- Morbid Obesity Center, Vestfold Hospital,
- HUNT – Trøndelag Health Survey, NTNU,
- AstraZeneca,
- Arctic Nutrition,
- Bio Me,
- Ness life,
- Pubgene,
Source: Helsenorge.no
Related article: How AI Artificial Intelligence could stimulate drug development